Evaluation of Telemedicine Efficacy in Diabetes Management: A Look Back at a Retrospective Study in an Urban Medically Underserved Population Area (UMUPA)
Alexander Oliver Chag 1
|
[1] University of Cape Town - Sudáfrica, alexanderoliverchag@hotmail.com, https://orcid.org/0009-0004-2730-6728
|
|
|
|
Copyright: © 2022 by the authors. This article is an open access article distributed under the terms and conditions of the Creative Commons
Received: 12 August, 2022
Accepted for publication: 26 September, 2022
|
ABSTRACT
This study assesses the effectiveness of telemedicine (TM) technology in comparison to traditional face-to-face (F2F) visits as an alternative healthcare delivery method for addressing diabetes within populations residing in urban medically underserved areas (UMUPAs). Electronic patient health records (ePHR) of individuals with type 2 diabetes mellitus (T2DM) were retrospectively examined from January 1, 2019, to June 30, 2021. Multiple linear regression models revealed that T2DM patients with uncontrolled diabetes using TM exhibited similar outcomes to those with traditional visits in reducing hemoglobin (HbA1c) levels.The type of healthcare service significantly influenced HbA1c % values, as evidenced by the regression coefficient for TM (vs. F2F) indicating a significant negative association (B = −0.339, p < 0.001). This suggests that patients utilizing TM were likely to have, on average, 0.34 lower HbA1c % values compared to those opting for F2F visits. Additionally, the regression coefficient for female (vs. male) gender demonstrated a positive association (B = 0.190, p < 0.034), revealing that female patients had HbA1c % levels 0.19 higher than their male counterparts. Age (B = −0.026, p < 0.001) emerged as a significant predictor of HbA1c % levels, with a decrease of 0.026 HbA1c % for each year increase in age.In terms of demographic factors, Black adults (B = 0.888, p < 0.001) were statistically more likely to exhibit 0.888 higher HbA1c % levels on average compared to White adults.
Keywords: Telemedicine; Diabetes Management; Retrospective Study; Medically Underserved Population
|
||
Evaluación de la Eficacia de la Telemedicina en el Manejo de la Diabetes: Un Vistazo a un Estudio Retrospectivo en un Área Urbana con Población Médicamente Desatendida (UMUPA)
RESUMEN
Este estudio evalúa la efectividad de la tecnología de telemedicina (TM) en comparación con las visitas tradicionales cara a cara (F2F) como un método alternativo de prestación de servicios de salud para abordar la diabetes en poblaciones que residen en áreas urbanas médicamente desatendidas (UMUPAs). Los registros electrónicos de salud de pacientes (ePHR) con diabetes mellitus tipo 2 (T2DM) fueron examinados retrospectivamente desde el 1 de enero de 2019 hasta el 30 de junio de 2021. Los modelos de regresión lineal múltiple revelaron que los pacientes con T2DM y diabetes no controlada que utilizaban TM mostraban resultados similares a aquellos con visitas tradicionales en la reducción de los niveles de hemoglobina (HbA1c). El tipo de servicio de atención médica influyó significativamente en los valores de HbA1c %, como lo evidenció el coeficiente de regresión para TM (vs. F2F), que indicaba una asociación negativa significativa (B = -0.339, p < 0.001). Esto sugiere que los pacientes que utilizaban TM probablemente tenían, en promedio, valores de HbA1c % 0.34 más bajos en comparación con aquellos que optaban por visitas F2F. Además, el coeficiente de regresión para el género femenino (vs. masculino) mostró una asociación positiva (B = 0.190, p < 0.034), revelando que las pacientes femeninas tenían niveles de HbA1c % 0.19 más altos que sus contrapartes masculinas. La edad (B = -0.026, p < 0.001) surgió como un predictor significativo de los niveles de HbA1c %, con una disminución de 0.026 HbA1c % por cada aumento de año en la edad. En cuanto a los factores demográficos, los adultos afroamericanos (B = 0.888, p < 0.001) eran estadísticamente más propensos a mostrar niveles de HbA1c % 0.888 más altos en promedio en comparación con los adultos blancos.
Palabras clave: Telemedicina; Manejo de la Diabetes; Estudio Retrospectivo; Población Médicamente Desatendida.
INTRODUCTION
The United States (US) grapples with a high incidence of diabetes, impacting over 38 million individuals, constituting around 10.5% of the population, with 29 million diagnosed cases and an additional 9 million undiagnosed [1]. Diabetes stands as the seventh leading cause of mortality in the US [1,2], with cardiovascular disease being the primary contributor [3]. In 2017, the estimated medical expenses for diagnosed diabetes reached USD 327 billion, encompassing both direct and indirect costs [2]. According to the World Health Organization (WHO), diabetes has ascended to the top 10 causes of global mortality, witnessing a 70% surge since 2000 [1]. The mortality rate among males has experienced an 80% increase [2]. Globally, the prevalence of diabetes has nearly doubled from 1980, escalating from 4.7% (108 million) to 8.5% (422 million) among adults in 2012 [3,4]. The rise in diabetes prevalence has been more rapid in low- and middle-income countries compared to high-income countries over the past decade [3,4]. The overall mortality rate of 43% among individuals under the age of 70 is primarily attributed to elevated blood sugar levels, particularly prevalent in low- and middle-income countries [3,4]. Elevated blood glucose levels have contributed to a global mortality rate of 2.2 million people, increasing the risks of cardiovascular and other diseases [3,4]. The stark statistics on the diabetes epidemic in the US and globally underscore the imperative need for this study.
Diabetes management and clinical care encounter challenges related to healthcare access, especially for high-risk groups [5], often resulting in debilitating health outcomes compounded by adverse socio-economic consequences for the general population [5,6]. The existing healthcare system in the United States (US) predominantly operates in a face-to-face (F2F) mode of care, necessitating patients to physically visit a facility, such as a healthcare provider’s office or clinic, to address their healthcare needs [7,8]. Traditional F2F visits were the predominant healthcare delivery service before the advent of the COVID-19 pandemic [9]. However, F2F healthcare services presented significant obstacles for vulnerable populations, particularly during the pandemic [8,10]. Vulnerable populations, limited to F2F visits for healthcare services, face a substantial health threat that could impede their ability to receive essential, life-saving, and timely treatment [10,11] for effective disease management [8]. Key factors for effectively managing diabetes include the timing of receiving care and the ability to access healthcare services [10,11].
The failure to initiate or sustain therapy, delays in treatment, and missed appointments are recognized as therapeutic or clinical inertia [12–14], often resulting in sustained high HbA1c glycemic levels, leading to micro- and macrovascular consequences [13–16]. Microvascular consequences involve small blood vessels, such as capillaries, while macrovascular consequences encompass large blood vessels like arteries and veins, resulting in severe medical conditions [16,17] arising from uncontrolled HbA1c levels. When individuals encounter barriers to healthcare services, a series of events typically unfolds, leading to the postponement or avoidance of medical care services [8], complicating disease management and contributing to adverse health outcomes [16–18].
Telehealth, TM, telemonitoring, remote monitoring, mobile (mhealth), and electronic health (ehealth), telemetric interventions, and virtual encounters are terms commonly used to describe informatics technologies [8,19]. The American Telemedicine Association (ATA) draws a distinction between TM and telehealth [19]. Telehealth and TM are often used interchangeably to refer to the exchange of medical information for healthcare delivery services when providers and patients are separated by distance and cannot meet in person [8,19]. TM is usually linked with direct remote patient "clinical" services, while telehealth encompasses a broader range of health-related services, including education and remote monitoring [19].
TM interactions may involve provider-to-patient, provider-to-provider, and patient-to-ancillary services (such as health coaching, technicians, and web-based interactive modules) [19]. TM encounters are categorized as synchronous, asynchronous, and continuous remote patient monitoring (RPM) [19]. Synchronous communication is live, real-time, and direct (audio-based—mobile or landline phones, or video-internet-based) [19]. Asynchronous communication, also referred to as store and forward (SF) communication, involves previously uploaded medical data used for future transmission [19]. This study specifically focuses on synchronous TM encounters, defined as "real-time" provider-to-patient communications using audio-based methods, i.e., mobile or landline phones, or video-internet-based methods [8,19].
The limited number of US-based research articles highlights the necessity for additional studies on this critical topic. Despite the global expansion of TM utilization, few studies have been conducted to showcase its effectiveness in diabetes management, with the potential for improving healthcare access among marginalized populations [8].
Therefore, this study is particularly pertinent in contributing to research aimed at assessing the effectiveness of interactive, synchronous TM as an alternative resource for healthcare delivery and patient care among marginalized populations [8]. The possibility of extending TM technology to individuals residing in medically underserved areas (MUAs), where chronic disease rates are high and access to healthcare services is inadequate, holds promise for alleviating health burdens, enhancing quality of life, and reducing medical costs [8].
As per the Department of Health and Human Services (HHS), distinct characteristics differentiate underserved and vulnerable groups within marginalized communities [20]. Populations classified as underserved generally share one or more traits, such as receiving fewer healthcare services, encountering multiple barriers (financial, cultural, or linguistic) when accessing essential healthcare services, lacking familiarity with the healthcare system delivery process, or residing in areas with a shortage of healthcare facilities and providers [20]. Vulnerable populations commonly exhibit higher risk factors for health issues or pre-existing conditions, limited options for livelihood (financial, educational, or housing), a lack of access to transportation services, and experiences of discrimination [20]. The population under consideration in this study falls into both the vulnerable and underserved categories [8].
The COVID-19 pandemic led to significant morbidity and mortality rates, overwhelming the US healthcare system [8] and restricting access to face-to-face (F2F) healthcare services for patients [20,21]. This situation propelled telemedicine (TM) technology to the forefront as an alternative healthcare delivery platform [8,21–23]. Consequently, TM technology became a crucial driver and instrument for change in the 21st-century healthcare delivery system [23], aiding in slowing the spread of the virulent COVID-19 disease [8,22,23]. Informatics technology, particularly TM, emerged as an indispensable component of healthcare delivery services in the US [8]. TM became an essential, life-saving means of reducing healthcare access barriers, offering options for individuals who would otherwise lack timely and adequate medical treatment [8].
Telehealth/TM has evolved into an essential core curriculum for health and medical informatics, recognized by the Journal of American Medical Informatics [24]. The curriculum aims to train healthcare professionals in utilizing TM informatics technology to expand distance-based healthcare delivery services, thereby improving access to marginalized communities [24].
Closing health equity gaps among vulnerable communities and addressing healthcare access barriers pose some of the most challenging issues for public health and the US healthcare systems [25]. While literature extensively documents barriers to healthcare access among racial and ethnic populations [7,25], there is limited evidence of successful interventions providing feasible solutions for populations residing in Urban Medically Underserved Population Areas (UMUPAs) [8], often disproportionately affected by social determinants of health (SDoH) [8,25,26]. According to the CDC, medically underserved areas (MUAs) are characterized by social determinants of health factors (SDoH) and are primary contributors to health challenges, restricting access to healthcare services [8,25–27].
Hence, this research delved into multiple studies to explore alternative methods for addressing the health equity gap among underserved/vulnerable populations with T2DM. The investigations analyzed numerous systematic reviews (SRs), meta-analyses (MAs), randomized control trials (RCTs), and qualitative studies from various geographical regions, countries, and time periods [8]. These studies consistently reported that TM is comparable to traditional visits in terms of effectiveness in reducing HbA1c % levels in patients with T2DM [28–30]. Encompassing diverse populations, these studies assessed the effectiveness of TM compared to traditional face-to-face visits for diabetes management and HbA1c % levels. The search covered reputable journals such as the Journal of Medical Internet Research [28], the World Journal of Diabetes [29], and the Informatics for Diabetes Education and Telemedicine (IDEATel) [30], all indexing comprehensive, archival studies published over several years [8].
In 2021, the Journal of Medical Internet Research (JMIR) conducted an extensive 12-year (2008–2020) systematic literature search on the effectiveness of telemedicine (TM) interventions in managing type 2 diabetes (T2DM) [28]. The study focused on TM communications between healthcare providers and patients, including both synchronous ("audio/video") [19] and asynchronous ("email, text messaging, and internet/web-based platforms") [19] methods for diabetes management and glycemic control [28]. The JMIR literature search encompassed 99 studies, involving 82,000 cases, 16,000 patients, and 7 countries. The results revealed an average decrease in HbA1c of 1.15%, with a mean HbA1c value of 6.95% [28].
The World Journal of Diabetes conducted a review in 2021, analyzing 43 meta-analyses (MAs) synthesizing randomized control trials (RCTs) spanning 31 years (1989–2020). The report highlighted a significant reduction in HbA1c levels (−0.486%) by extracting data from the difference in mean HbA1c levels [29].
Long-term RCTs for TM case management, undertaken by the Informatics for Diabetes Education and Telemedicine (IDEATel), found that patients maintained an improvement in HbA1c levels of 0.29% over 5 years [30]. The IDEATel study targeted adults over 55 years, ethnically diverse (African-American and Hispanic), fluent in English or Spanish, Medicare beneficiaries with T2DM, and residing in federally designated Medically Underserved Areas (MUAs) or Health Professional Shortage Areas (HPSAs) of New York State [30].
This study explores an alternative to traditional face-to-face (F2F) healthcare, utilizing synchronous TM communications [19]. This approach has the potential to offer a life-saving, limb-saving, and cost-saving strategy for diabetes management [13,17] by enhancing access to care services for marginalized populations [8]. In this context, "access" refers to the type of healthcare service (TM or F2F) and its suitability in meeting the needs of Urban Medically Underserved Population Areas (UMUPA) residents concerning access to medical treatment [8].
MATERIALS AND METHODS
This study conducted a distinctive analysis of retrospective electronic patient health records covering the period from January 1, 2019, to June 30, 2021, focusing on patients with type 2 diabetes mellitus (T2DM) exhibiting both uncontrolled diabetes and prediabetes. The research employed a quantitative study design.
Ethical Approval
The study adhered to the principles of the Declaration of Helsinki and received approval from the Institutional Review Boards (IRBs)–Ethics Committees of Georgia Southern University (GSU) and the University of Florida (UF) for studies involving human subjects. The study's protocol obtained approval from the UF Health System IRB (#IRB202102147) and GSU IRB (# H22O44). Exempt status for chart reviews was granted for the secondary collection of electronic patient health record (PHR) data. The archival, retrospective data were initially collected by UF Health Electronic Health Records (EHR) for "healthcare operations" or "public health activities and purposes" under "45 CFR 164.512(b)" and "45 CFR 164.501." UF IRB 01 designated the study as secondary research, waiving the need for consent. The research did not involve participants enrolled in experimental protocols. Patient identifiable information was not obtained, and data collection occurred anonymously through a third party.
Sample
The study sample comprised patients with type 2 diabetes from the Commonwealth Family Medicine Clinic (CFMC) exhibiting uncontrolled diabetes (≥8.0%) and prediabetes (≥5.7–6.8%). The assessment of diabetes care effectiveness was based on changes in HbA1c % levels, comparing telemedicine (TM) with the traditional face-to-face (F2F) mode of care. Patients with managed or controlled diabetes were excluded from the analyses due to the relatively stable levels of HbA1c %. Hence, they were not the focal point of this investigation.
The majority of patients empaneled in this study reside in an urban medically underserved area (UMUPA) within a sub-county of Jacksonville, Florida—Duval County, known as the "Urban Core" or Health Zone 1 (HZ 1). The population in HZ 1 is predominantly African American/Black (80%), with 49.5% relying on Medicaid as their medical insurer [31]. Residents in HZ 1 face significant diabetes-related health challenges [32] linked to social determinants of health (SDoH) factors, including high rates of obesity and poverty, the prevalence of food deserts, lower socioeconomic status, and literacy deficiencies [31,32]. In 2019, Duval County ranked third in Florida for the hospitalization rate due to diabetes-related complications among Blacks, with the eighth-highest count (33,842) across all demographic groups in the state [33,34].
Study Variables
The sociodemographic covariates in this study were operationalized to include the patient's age, birth gender, race, ethnicity, provider type/title, medical insurer, appointment status, and the five-digit zip code, which was subsequently converted into regions identified as Health Zones (HZs). Due to the limited patient populations in these HZs, data aggregation was necessary, leading to their recoding into four groups based on geographic proximity.
Age: This variable represents the age in years at the date of the visit encounter.
Gender: The birth gender of the research participants was operationalized and recoded into two categories: male and female. Male serves as the reference category when comparing with the female category.
Race/Ethnicity: This patient demographic variable was operationalized into three groups, with codes as follows: 0 = White, 1 = African American/Black, and 2 = Asian/other. The reference category is White (coded as 0) when comparing with the other categories.
Medical insurer type: This variable was determined based on the patient's primary medical insurer/payer for the healthcare visit at the time of service. It was categorized into three groups and recoded as follows: 0 = Medicare, 1 = Medicaid, and 2 = Private/other. The reference category is Medicare (coded as 0) when comparing with the other categories. Note: The US federal health insurance programs Medicare and Medicaid are administered by the Centers for Medicare & Medicaid Services (CMS), with Medicare catering to individuals 65 and older or those with specific disabilities or conditions, and Medicaid assisting individuals with limited resources and low incomes in covering medical expenses [35].
Health Zones (HZs) in Duval County identified by five-digit zip codes: The HZ variable was operationalized to represent populations residing in different regions of Duval County, initially coded as HZs 1 through 6. These regions were labeled as follows: HZ 1–Urban Core (MUA), HZ 2–Greater Arlington, HZ 3–Southeast, HZ 4–Southwest (SW), HZ 5–Rural–Outer Rim (MUA), and HZ 6–Beaches. Subsequently, the HZs were reorganized, given new names based on geographical location or proximity, and adjusted for small population sizes. The condensed, recoded regions were named as follows: HZ MUA, HZ SW, HZs Outer Duval County, and Out of Area.
The HZ MUA, comprising 60% of the total patient population and located in medically underserved areas of Duval County, combines two HealthZones: 1 and 5 [HZ 1–Urban Core (n = 52%) and 5-Rural–Outer Rim (n = 8%)]. * The HZ SW remains in its own category, representing 32% of the clinic's population. The HZs in Outer Duval County encompass 12% of the total clinic population and include three HealthZones: 2, 3, and 6 [HZ 2–Greater Arlington (n = 3%), HZ 3–Southeast (n = 0.8%), and HZ 6–Beaches (n = 0.5%)]. Out of Area patients make up 4% of the clinic's patient pool and live in another state or a non-local region of Florida, thus not being assigned to any HZ and being omitted. The majority of empaneled patients in the Commonwealth Family Medicine Clinic (CFMC) reside in a Duval County sub-county identified as HZ1, the Urban Core. When comparing with other covariates, the HZ SW serves as the reference category. Note: * denotes medically underserved areas.
Provider Type (Title): This variable represents the title/type of the provider conducting the patient visit, categorized as Medical Doctor (MD), Nurse Practitioner (NP), and Physician’s Assistant (PA). The NP serves as the reference category, with a code of (0) when compared to the other categories.
Medical Appointments: The type of healthcare service was either Telemedicine (TM) or Face-to-Face (F2F) visits. TM appointments involved synchronous consultations with a healthcare professional using real-time audio/video communication [8,19].
Statistical Methods
The initial steps involved cleaning, recoding, and scrutinizing the primary dataset for missing data and outliers. After data examination, imputation was conducted for 7 missing lab values, and 21 patients were excluded due to not meeting the criteria or having appointments outside of CFMC. The final baseline cohort consisted of 366 patients with 3749 clinic visits. The subsequent step was the identification and subdivision of the primary dataset into separate subsets based on patient HbA1c % levels for those with uncontrolled diabetes (≥8.0%) and prediabetes (≥5.7–6.8%), as well as the type of appointment (TM or F2F).
Analyses were performed using multiple linear regression (MLR) models for patient visits with uncontrolled diabetes and prediabetes, examining the relationship between HbA1c % levels and covariates (age, gender, race, HZ, medical insurance, healthcare service type, and provider type/title). Data were summarized using frequency and percentages for categorical data.
Results Comparing Patient HbA1c % Levels Using TM and F2F Healthcare
Descriptive Statistics for Patients with Uncontrolled Diabetes and Prediabetes
Table 1 displays frequencies and percentages for the categorical variables of all patients with uncontrolled diabetes (n = 1685) and prediabetes visits (n = 634). Demographics with the highest numbers and percentages for patients with uncontrolled diabetes included Black individuals (n = 1234, 73.23%), non-Hispanic individuals (n = 1668, 98.99%), females (n = 1014, 60.18%) residing in medically underserved areas (MUAs–HZ 1 and HZ 5) (n = 917, 54.42%). The majority of visits were with NPs (n = 1087, 64.51%). Medicaid (n = 698, 41%) was the most prevalent type of medical insurance. Both types of healthcare visits were used equally, with 843 being F2F visits (50.03%) and 842 patients utilizing TM appointments (49.97%).
Table 1. Descriptive Statistics for Patient Visits with Uncontrolled Diabetes and Prediabetes in Type 2 Diabetes Mellitus (T2DM).
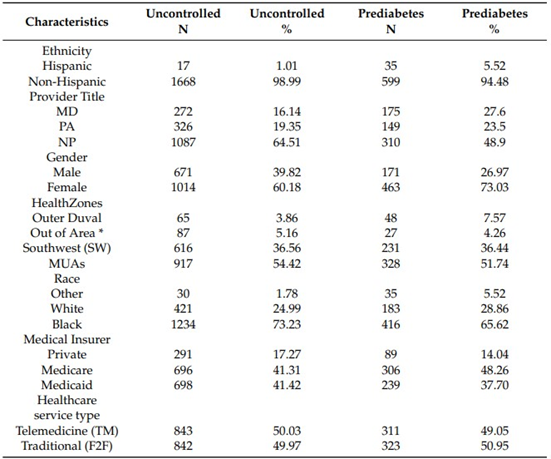
*Outside the geographical scope of a HealthZone region
The demographic groups with the highest counts and percentages of patients diagnosed with prediabetes included individuals who were Black (n = 416, 66%), Non-Hispanic (n = 599, 94.5%), female (n = 463, 73%), and residing in medically underserved areas (MUAs) (n = 328, 52%). The Nurse Practitioner (NP) had the highest number of visits with this patient group (n = 310, 49%). Healthcare service utilization was nearly balanced between Face-to-Face (F2F) appointments (n = 323, 50.95%) and Telemedicine (TM) appointments (n = 311, 49.05%). Medicare was the predominant type of medical insurance (n = 306, 48.3%). The average age of these patients was 59.4 years (SD = 11.65).
Tables
Patients with Type 2 Diabetes Mellitus (T2DM) Uncontrolled Diabetes Visits
The Multiple Linear Regression (MLR) model for patients with T2DM experiencing uncontrolled diabetes visits examined the levels of HbA1c % along with covariates (age, gender, race, provider type/title, healthcare service, medical insurer, and Health Zones), revealing significance (Table 2) F(8, 1676) = 25.781, p < 0.001, R² = 0.105. The R² for the overall model indicates an effect size of 0.105, suggesting that approximately 10.5% of the variability in HbA1c % levels is accounted for by the covariates in the model.
Table 2. Multiple Linear Regression Model Analyzing HbA1c % Levels and Covariates
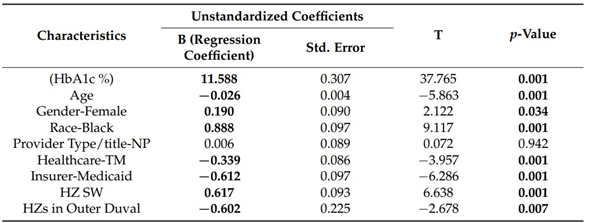
Note: MLR model was significant F(8, 1676) = 25.781, p <0.001, R2 = 0.105. Bold indicates statistical significance.
Unstandardized Regression Equation: HbA1c = 11.588 + age (−0.026) + Gender-Female (0.190) + Race-Black
(0.888) + NP (0.006) + Healthcare service-TM (−0.339) + Medicaid (−0.612). + HZ SW* (0.617) + HZ Outer
Duval (−0.602).
The outcomes of the Multiple Linear Regression (MLR) model for patients with uncontrolled diabetes visits due to Type 2 Diabetes Mellitus (T2DM) were highly significant at p < 0.001 (Table 2). The utilization of Telemedicine (TM) as the healthcare service significantly correlated with lower HbA1c % values, as indicated by the regression coefficient for TM (vs. F2F), which demonstrated a noteworthy negative association (B = −0.339, p < 0.001). This implies that, after accounting for other factors in the model, patients opting for TM were expected to have, on average, 0.34 lower HbA1c % values compared to those choosing Face-to-Face (F2F) visits. The regression coefficient for the female gender (vs. male) exhibited a significant positive association (B = 0.190, p < 0.034), suggesting that female patients tended to have 0.19 higher HbA1c % levels than their male counterparts.
Age (B = −0.026, p < 0.001) emerged as a significant predictor of HbA1c % levels, indicating a decrease of 0.026 HbA1c % for each year increase in age. Black adults (B = 0.888, p < 0.001) were statistically more likely to have, on average, 0.888 higher HbA1c % levels compared to White adults, considering other covariates in the model. The Health Zone (HZ) SW (B = 0.617, p < 0.001), in comparison to the Medically Underserved Areas (MUAs), was, on average, more likely to exhibit 0.617 higher HbA1c % levels.
Outer Duval County (B = −0.602, p < 0.007) was a significant predictor when compared to MUAs, indicating that a patient in Outer Duval County was, on average, likely to have 0.602% lower HbA1c % levels. The medical insurer Medicaid (B = −0.612, p < 0.001) was also a significant predictor, suggesting that patients with Medicaid, in comparison with Medicare, had, on average, 0.612 lower HbA1c % levels. The type of healthcare provider, Nurse Practitioner (NP) (B = 0.006, p = 0.943), was not statistically significant when compared with other healthcare providers. The detailed results of the MLR model for T2DM patients with uncontrolled diabetes – HbA1c % levels and covariates, including gender, age, race, healthcare service type, provider type, HZs, and medical insurer, are presented in Table 2.
Patients with Prediabetes Visits
The MLR model for patients with prediabetes visits scrutinized the HbA1c % levels and covariates (age, gender, race, provider type/title, healthcare service, medical insurer, and HZs), indicating significance (Table 3) F(8, 634) = 8.842, p < 0.001, R² = 0.100. The R² for the overall model suggests an effect size of 0.100, signifying that approximately 10% of the variability in HbA1c % levels can be explained by the covariates in the model.
Table 3 presents the results of the Multiple Linear Regression, examining the association between HbA1c % levels and various covariates.
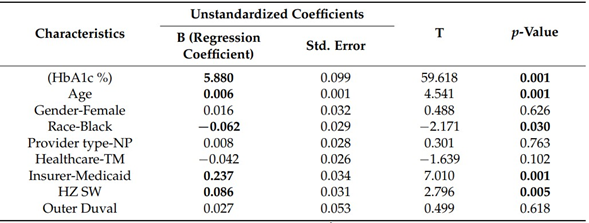
Note: MLR model was significant F(8, 634) = 8.842, p < 0.001, R2 = 0.100. Bold indicates statistical significance at
p < 0.05. Unstandardized Regression Equation: HbA1c = 5.880 + age (0.006) + gender-female (0.016) + Black (−0.062)
+ HZ SW (0.086) + HZ Outer Duval* (0.027) + Healthcare service-TM (−0.042) + NP (0.008) + Medicaid (0.237).
The age of the patients (B = 0.006, p < 0.001) emerged as a significant predictor, indicating that, on average, each additional year of age is associated with a 0.006 increase in HbA1c % levels. The race category for Black adults (B = −0.062, p = 0.030) also exhibited a statistically significant association with the outcome compared to White adults, suggesting that Black adults, on average, tended to have HbA1c levels lower by 0.062% than their White counterparts. Patients residing in HZ SW (B = 0.086, p = 0.005) were found to have a 0.086 higher HbA1c % compared to those in HZ MUAs. The type of medical insurer Medicaid (B = 0.237, p < 0.001) was identified as a significant predictor of HbA1c compared with Medicare, implying that patients with Medicaid were likely to have 0.237 higher HbA1c % levels than those with Medicare.
After adjusting for other covariates in this model, the variable of gender (B = 0.016, p = 0.626) did not show a statistically significant association with HbA1c. Similarly, the healthcare service type TM (B = −0.042, p = 0.102) did not exert a significant effect on HbA1c % levels when compared to F2F visits. The HZ Outer Duval County (B = 0.027, p = 0.618), when compared with MUAs, did not demonstrate a significant association with HbA1c levels. The NP provider type (B = 0.008, p = 0.763) was not found to be a significant factor in predicting HbA1c compared to other healthcare providers.
In summary, the MLR model for patients with uncontrolled diabetes indicated a significant negative association with age, healthcare service type TM, medical insurer-Medicaid, and Outer Duval County. Positive associations with HbA1c % levels were observed for the variables of female gender, Black race, and HZ SW, while the provider type was not statistically significant. The MLR model for patients with prediabetes indicated a significant negative association of race with HbA1c % levels, and positive associations were observed for the medical insurer Medicaid and HZ SW. Gender, healthcare service type, HZs in Outer Duval County, and provider type were not statistically significant. Refer to Tables 2 and 3 for detailed results from the MLR model, focusing on patients with uncontrolled diabetes and prediabetes, respectively, and their HbA1c % levels and covariates [8].
The predictive influence of patient age (B = 0.006, p < 0.001) was established as noteworthy, signifying that, on average, each additional year of age corresponded to a 0.006 elevation in HbA1c % levels. The category representing Black adults (B = −0.062, p = 0.030) retained its significant association with the outcome compared to White adults, suggesting that, on average, Black adults were expected to have HbA1c levels lower by 0.062% than their White counterparts. Patients residing in HZ SW (B = 0.086, p = 0.005) were prone to experiencing a 0.086 increase in HbA1c %, relative to those in HZ MUAs. The medical insurer Medicaid (B = 0.237, p < 0.001) emerged as a pivotal predictor of HbA1c, indicating that Medicaid beneficiaries were likely to exhibit 0.237 higher HbA1c % levels compared to those with Medicare coverage.
Upon meticulous consideration of other covariates in this model, the gender variable (B = 0.016, p = 0.626) did not demonstrate a significant correlation with HbA1c. Similarly, the healthcare service type TM (B = −0.042, p = 0.102) did not manifest a notable impact on HbA1c % levels when contrasted with traditional F2F visits. The geographical designation of HZ Outer Duval County (B = 0.027, p = 0.618), in contrast to MUAs, did not exhibit a statistically significant connection with HbA1c levels. Furthermore, the provider type NP (B = 0.008, p = 0.763) did not emerge as a statistically significant factor in predicting HbA1c when compared to other healthcare provider categories.
Summary
In summation, the multivariate linear regression (MLR) model for patients with uncontrolled diabetes unveiled a significant negative association involving age, healthcare service type TM, medical insurer Medicaid, and Outer Duval County. Conversely, positive associations were observed for variables such as female gender, Black race, and HZ SW, whereas the provider type did not attain statistical significance. For patients with prediabetes, the MLR model indicated a significant negative association with race concerning HbA1c % levels, while positive associations were observed for medical insurer Medicaid and HZ SW. In contrast, gender, healthcare service type, HZs in Outer Duval County, and provider type did not exhibit statistical significance. Detailed results of the MLR model for patients with uncontrolled diabetes and prediabetes are presented in Tables 2 and 3, respectively, focusing on HbA1c % levels and covariates [8].
DISCUSSION
The focal point of this study was to explore the management of diabetes among patients diagnosed with Type 2 Diabetes Mellitus (T2DM) residing in urban medically underserved areas (UMUPAs), utilizing both Telemedicine (TM) and Face-to-Face (F2F) healthcare services [8]. Populations situated in Medically Underserved Areas (MUAs) and UMUPAs encounter substantial personal and systemic obstacles in accessing adequate healthcare services [8]. These challenges are particularly problematic for individuals with chronic illnesses, often resulting in complications in disease management and unfavorable health outcomes [7,36]. The attainment of optimal glycemic control, as measured by managing HbA1c % levels, is crucial for individuals with diabetes to mitigate potential micro- and macrovascular complications [16,17,37].
At the time of this research, there was a dearth of US-based studies examining the effectiveness of TM/F2F visits in diabetes management and HbA1c % levels [8]. The limited number of US-based research articles underscored the necessity for additional investigations into this critical topic [8]. This study stood out in several aspects, employing a retrospective quantitative study design and utilizing regression models to capture unique real-time Personal Health Record (PHR) data [8]. It uniquely scrutinized the health records of patients with both prediabetes and uncontrolled T2DM within a single medical clinic, all residing in UMUPAs, who had appointments using both TM technology and F2F modalities [8]. The research population exhibited one of the highest rates of chronic diseases, hospitalizations, and Emergency Room (ER) visits related to diabetes in the state of Florida [31,32,34]. In contrast to previous studies relying on systematic reviews and meta-analyses, this research drew on original data extracted from patient health records [8].
The study covered the period from January 2019 to June 2021, encompassing pre-Covid and Covid years, during which TM utilization rates among patients increased. Patients in this specific clinic with T2DM emerged as the highest TM utilizers [8]. Patients had the flexibility to opt for either TM or F2F visits, with both visit types being mandatory for inclusion in the study during the specified period [8]. The subjective reasons influencing patients' choices of healthcare visits can only be speculative within the scope of this research design, which is primarily quantitative and retrospective. This design imposes limitations on the type of data that researchers can gather and does not account for confounding variables. The patient population with prediabetes was comparatively smaller than that of patients with T2DM, and individuals with prediabetes may have distinct perspectives on disease management compared to T2DM patients.
While there were no comparable US-based studies at the time of this research, the final results aligned with findings from other studies [8,28–30]. The outcomes established a significant association between the utilization of TM, in comparison to traditional visits, and lower HbA1c % levels (p < 0.001) in patients with uncontrolled T2DM, indicating the efficacy of TM as a diabetes management tool [8]. Notably, there was no significant association between patients with prediabetes and the utilization of TM for healthcare services (p = 0.102), potentially due to the limited number of patients available for analysis.
Several limitations were inherent in the study design, restricting the precision of data endpoints reflecting changes in HbA1c % values at specific time intervals. The extraction of retrospective, secondary data initially collected for clinical practice posed challenges for research purposes. External factors, such as the data being collected both before and during the COVID-19 pandemic, lifestyle, availability of healthy food options, physical activity, social support, self-efficacy, relational dynamics, medications, stress, and mental health challenges, may have influenced outcomes [8].
Effective management of diabetes helps prevent future complications related to uncontrolled HbA1c levels. The reduction in HbA1c levels is pivotal and can mitigate diabetes-related deaths and micro- and macrovascular complications [15–17] in patients with T2DM [37]. A seminal study conducted for the UK Prospective Diabetes Study (UKPDS) revealed that a 1% reduction in mean HbA1c is associated with a 21% reduction in diabetes-related deaths and a 37% reduction in microvascular complications in T2DM patients [16]. Future research endeavors could incorporate a mixed methods approach, combining qualitative components with the current quantitative approach to yield findings more applicable to patient care [8]. In a non-pandemic environment, a more in-depth assessment of patient perspectives, such as technology experience and details of their healthcare visit, would be feasible [8]. Further studies on prediabetes care are imperative to gain insights into how TM may function as a preventative strategy, mitigating the future incidence of T2DM.
CONCLUSIONS
In conclusion, this study contributes novel empirical data to the realm of health informatics, specifically aimed at enhancing healthcare services, particularly for populations facing significant barriers to access. The investigation focused on leveraging telemedicine (TM), an information technology, to manage Type 2 Diabetes Mellitus (T2DM) in medically underserved areas with restricted access to healthcare services [8].
The analysis delved into patients' HbA1c % levels across the diabetes spectrum, ranging from the initial stages of diabetes development (prediabetes) to the advanced stage (uncontrolled diabetes) [8]. The primary objective was to evaluate the effectiveness of TM in comparison to Face-to-Face (F2F) visits in diabetes care. Patients in the prediabetes and uncontrolled diabetes categories represent a crucial stage in terms of clinical outcomes [8]. Ensuring timely prevention and intervention is paramount in arresting the progression of elevated glycemic levels, consequently reducing the risk of complications [8,37].
TM equips practitioners with real-time data through technology, enabling continuous monitoring of patients and offering an efficient avenue for accessing timely and potentially life-saving healthcare services. Evidence suggests that enhancing healthcare access for individuals with T2DM can mitigate complications in disease management, subsequently lowering morbidity and mortality rates [37].
To effectively address the escalating global diabetes epidemic, healthcare providers must transition from conventional disease-oriented tertiary care to implementing preventative care solutions. Identifying alternative, evidence-based, scalable interventions for healthcare services becomes imperative as a preemptive strategy to cater to the current and future health needs of the population [8].
The study's outcomes may also guide healthcare facilities and medical clinics in tailoring interventions using informatics technology to enhance care for patients with various chronic illnesses and alleviate health disparities among communities influenced by social determinants of health.
Despite the acknowledged limitations of the study, we anticipate that our research will stimulate future investigations. The uniqueness of this study, addressing a critically important and urgent topic in disease management, particularly in marginalized regions, may prompt further research endeavors.
BIBLIOGRAPHICAL REFERENCES
WHO. WHO Reveals Leading Causes of Death and Disability Worldwide: 2000–2019. Available online: https://www.who.int/news/item/09-12-2020-who-reveals-leading-causes-of-death-and-disability-worldwide-2000-2019 (accessed on 28 April 2021).
American Diabetes Association. Economic Costs of Diabetes in the U.S. in 2017. Diabetes Care 2018, 41, 917–928. [CrossRef]
Report of the First Meeting of the WHO Global Diabetes Compact Forum. 2021. Available online: https://www.who.int/publications/i/item/9789240045705 (accessed on 14 January 2023).
WHO. Int Fact Diabetes Sheet. Available online: https://www.who.int/news-room/fact-sheets/detail/diabetes (accessed on 5 May 2021).
CDC. Certain Medical Conditions and Risk for Severe COVID-19 Illness|CDC. Available online: https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html (accessed on 28 April 2021).
Adegunsoye, A.; Ventura, I.B.; Liarski, V.M. Association of Black Race with Outcomes in COVID-19 Disease: A Retrospective
Cohort Study. Ann. Am. Thorac. Soc. 2020, 17, 1336–1339. [CrossRef] [PubMed]
Braveman, P. Health Disparities and Health Equity: Concepts and Measurement. Annu. Rev. Public Health 2006, 27, 167–194.
[CrossRef]
Ward, L.A. Effectiveness of Telemedicine in Diabetes Management: A Retrospective Study in an Urban Medically Underserved
Population Area (UMUPA). Available online:
https://digitalcommons.georgiasouthern.edu/cgi/viewcontent.cgi?article=3706
&context=etd (accessed on 3 November 2022).
Temesgen, Z.M.; DeSimone, D.C.; Mahmood, M.; Libertin, C.R.; Varatharaj Palraj, B.R.; Berbari, E.F. Health Care After the
COVID-19 Pandemic and the Influence of Telemedicine. Mayo Clin. Proc. 2020, 95, S66–S68. [CrossRef]
CDC. Preventing Diabetes-Related Complications|Diabetes|CDC. Available online:
https://www.cdc.gov/diabetes/data/statistics-report/preventing-complications.html (accessed on 7 September 2021).
McElroy, J.A.; Day, T.M.; Becevic, M. The Influence of Telehealth for Better Health Across Communities. Prev. Chronic Dis. 2020,
17, 200254. [CrossRef]
. Andreozzi, F.; Candido, R.; Corrao, S.; Fornengo, R.; Giancaterini, A.; Ponzani, P.; Ponziani, M.C.; Tuccinardi, F.; Mannino, D.
Clinical inertia is the enemy of therapeutic success in the management of diabetes and its complications: A narrative literatura review. Diabetol. Metab. Syndr. 2020, 12, 52. [CrossRef] [PubMed]
Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes—2020|Diabetes Care. Available online: https://care.diabetesjournals.org/content/43/Supplement_1/S14 (accessed on 7 September 2021).
Pantalone, K.M.; Misra-Hebert, A.D.; Hobbs, T.M.; Ji, X.; Kong, S.X.; Milinovich, A.; Weng, W.; Bauman, J.; Ganguly, R.; Burguera,
B.; et al. Clinical Inertia in Type 2 Diabetes Management: Evidence From a Large, Real-World Data Set. Diabetes Care 2018, 41,
e113–e114. [CrossRef]
Cade, W.T. Diabetes-Related Microvascular and Macrovascular Diseases in the Physical Therapy Setting. Phys. Ther. 2008, 88,
1322–1335. [CrossRef]
Stratton, I.M. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35):
Prospective observational study. BMJ 2000, 321, 405–412. [CrossRef] [PubMed]
Informatics 2023, 10, 16 12 of 12
Hirakawa, Y.; Arima, H.; Zoungas, S.; Ninomiya, T.; Cooper, M.; Hamet, P.; Mancia, G.; Poulter, N.; Harrap, S.; Woodward,
M.; et al. Impact of Visit-to-Visit Glycemic Variability on the Risks of Macrovascular and Microvascular Events and All-Cause Mortality in Type 2 Diabetes: The Advance Trial. Diabetes Care 2014, 37, 2359–2365. [CrossRef]
Khunti, K.; Gomes, M.B.; Pocock, S.; Shestakova, M.V.; Pintat, S.; Fenici, P.; Hammar, N.; Medina, J. Therapeutic inertia in the treatment of hyperglycaemia in patients with type 2 diabetes: A systematic review. Diabetes Obes. Metab. 2018, 20, 427–437.
[CrossRef] [PubMed]
Telehealth Basics-ATA. Available online: https://www.americantelemed.org/resource/why-telemedicine/ (accessed on 2 September 2021).
DHS. Federally-Facilitated Marketplace Assister Curriculum Serving Vulnerable and Underserved Populations. Department of Health & Human Services Centers for Medicare & Medicaid Services Center for Consumer Information & Insurance Oversight;
2014:108. Available online:
https://mail.google.com/mail/u/0/#inbox/WhctKKXpSdCrPvRlSTHvtnfmSgRmFchWfGmFFvLsCgFKCVbzKrBCMgxLPjcmtncgpsJRlgG?compose=new&projector=1&messagePartId=0.1 (accessed on 25 June 2022).
Vilendrer, S.; Patel, B.; Chadwick, W.; Hwa, M.; Asch, S.; Pageler, N.; Ramdeo, R.; Saliba-Gustafsson, E.A.; Strong, P.; Sharp, C.
Rapid Deployment of Inpatient Telemedicine In Response to COVID-19 Across Three Health Systems. J. Am. Med. Inform. Assoc.
2020, 27, 1102–1109. [CrossRef] [PubMed]
Bashshur, R.; Doarn, C.R.; Frenk, J.M.; Kvedar, J.C.; Woolliscroft, J.O. Telemedicine and the COVID-19 Pandemic, Lessons for the Future. Telemed. E Health 2020, 26, 571–573. [CrossRef] [PubMed]
Sounderajah, V.; Patel, V.; Varatharajan, L.; Harling, L.; Normahani, P.; Symons, J.; Barlow, J.; Darzi, A.; Ashrafian, H. Are disruptive innovations recognised in the healthcare literature? A systematic review. BMJ Innov. 2021, 7, 208–216. [CrossRef]
[PubMed]
Demiris, G. Integration of Telemedicine in Graduate Medical Informatics Education. J. Am. Med. Inform Assoc. 2003, 10, 310–314.
[CrossRef] [PubMed]
About Social Determinants of Health (SDOH). Published 10 March 2021. Available online: https://www.cdc.gov/socialdeterminants/about.html (accessed on 23 April 2021).
.Walker, R.J.; Strom Williams, J.; Egede, L.E. Influence of Race, Ethnicity and Social Determinants of Health on Diabetes Outcomes.
Am. J. Med. Sci. 2016, 351, 366–373. [CrossRef]
. Klein, R.; Huang, D. Defining and Measuring Disparities, Inequities, and Inequalities in the Healthy People Initiative. National Center of Health Statistics NCHS-CDC. Available online:
https://www.cdc.gov/nchs/ppt/nchs2010/41_klein.pdf (accessed on July 2022).
Eberle, C.; Stichling, S. Effect of Telemetric Interventions on Glycated Hemoglobin A1c and Management of Type 2 Diabetes Mellitus: Systematic Meta-Review. J. Med. Int. Res. 2021, 23, e23252. [CrossRef]
De Groot, J.; Wu, D.; Flynn, D.; Robertson, D.; Grant, G.; Sun, J. Efficacy of telemedicine on glycaemic control in patients with type 2 diabetes: A meta-analysis. World J. Diabetes 2021, 12, 170–197. [CrossRef]
Shea, S.; Weinstock, R.S.; Teresi, J.A.; Palmas, W.; Starren, J.; Cimino, J.J.; Lai, A.M.; Field, L.; Morin, P.C.; Goland, R.; et al.
A Randomized Trial Comparing Telemedicine Case Management with Usual Care in Older, Ethnically Diverse, Medically Underserved Patients with Diabetes Mellitus: 5 Year Results of the IDEATel Study. J. Am. Med. Inform. Assoc. 2009, 16, 446–456.
[CrossRef]
Duval County, Florida|County Health Rankings & Roadmaps. Available online: https://www.countyhealthrankings.org/app/florida/2021/rankings/duval/county/outcomes/overall/snapshot (accessed on 23 April 2021).
U.S. Census Bureau QuickFacts: Duval County, Florida. Available online:
https://www.census.gov/quickfacts/fact/table/duvalcountyflorida/INC110219 (accessed on 10 October 2021).
Livingood, W.C.; Razaila, L.; Reuter, E.; Filipowicz, R.; Butterfield, R.C.; Lukens-Bull, K.; Edwards, L.; Palacio, C.; Wood, D.L.
Using multiple sources of data to assess the prevalence of diabetes at the subcounty level, Duval County, Florida, 2007. Prev.
Chronic Dis. 2010, 7, A108.
FLHealthCHARTS.com: Chronic Disease Data. Available online: https://flhealthcharts.com (accessed on 10 October 2021).
Difference between Medicare and Medicaid Insurance. Available online:
https://www.hhs.gov/answers/medicare-andmedicaid/what-is-the-difference-between-medicare-medicaid/index.html (accessed on 12 January 2023).
Canedo, J.R.; Miller, S.T.; Schlundt, D.; Fadden, M.K.; Sanderson, M. Racial/Ethnic Disparities in Diabetes Quality of Care: The Role of Healthcare Access and Socioeconomic Status. J. Racial Ethn. Health Disparities 2018, 5, 7–14. [CrossRef] [PubMed]
Viigimaa, M.; Sachinidis, A.; Toumpourleka, M.; Koutsampasopoulos, K.; Alliksoo, S.; Titma, T. Macrovascular Complications of Type 2 Diabetes Mellitus. Curr. Vasc. Pharmacol. 2020, 18, 110–116. [CrossRef] [PubMed]